Transfusions and Platelet Donations

What is platelet donation?
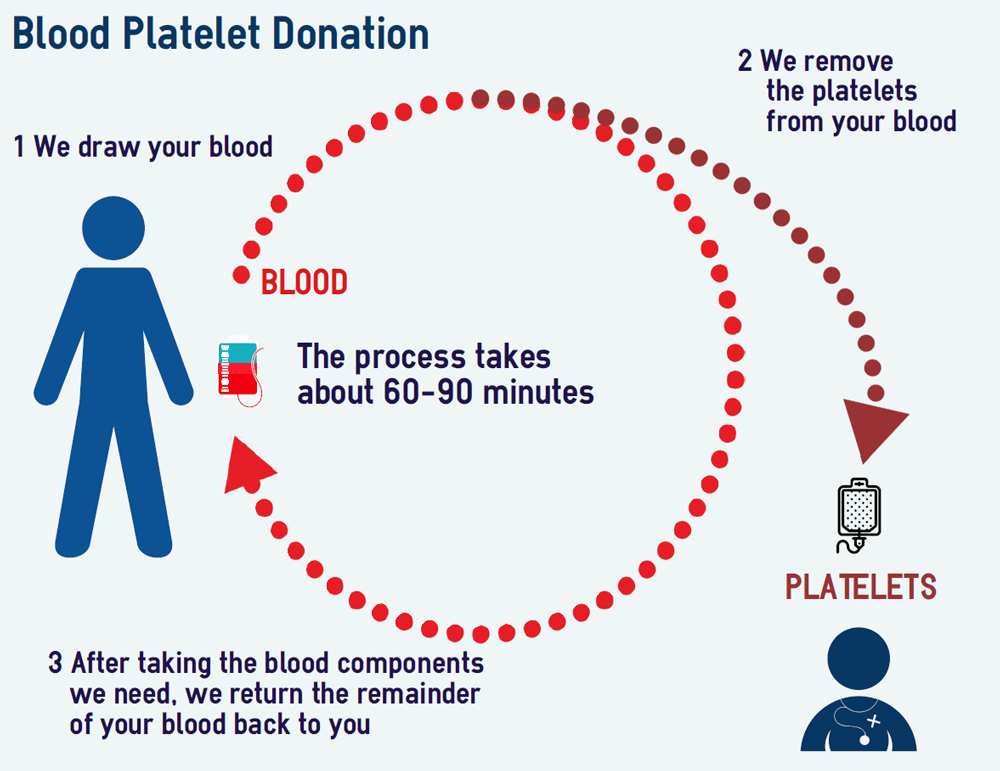
- Platelet donation is the process of extracting platelets from the blood of donors through a special procedure called “apheresis”.
- Platelets have a key role in stopping or preventing bleeding.
- Most platelet donations are given to patients who are unable to make enough platelets in their bone marrow. For example, patients with leukaemia or other cancers may have too few platelets as the result of their disease or treatment. Also after major surgery or extensive injury, patients may need platelet transfusions to replace those lost through bleeding.
- Platelets can only be stored for a few days, so platelet donors are asked to attend at least 8 – 10 times per year, up to a maximum of 24 times a year with a minimum interval between donations of 14 days.
- A platelet donation takes up to 90 minutes. You will be asked to undergo a Donor Health Check (as with blood donation) first and encouraged to have a short rest and drink afterwards. You can expect to the whole process to take up to 2 hours.
 How are platelets donated?
How are platelets donated?
- A cuff is placed around your arm, the skin cleaned, local anaesthetic may be injected and the donation needle inserted. Blood samples are taken at this stage for testing in the same way as whole blood donations.
- Additional tests carried out for platelet donors including checking your platelet count and determining your tissue type (so that your platelets can be matched to those of a particular patient if needed).
- While you are donating you will be monitored and cared for by qualified staff supervised by nurses. You can read, chat to the staff or relax and you will be offered refreshments. When the procedure is completed the needle will be removed and a dressing applied to the venepuncture site.
Who can donate platelets?
- Eligibility criteria in terms of age and health are the same for blood and platelet donors, but for platelet donation but your height and weight ratio has to be assessed to check your blood volume.
- There is one additional medication rule: you cannot donate platelets if you have taken aspirin, aspirin-containing medications, piroxicam or nonsteroidal anti-inflammatory drugs, such as Ibuprofen in the last 48 hours. This is because these drugs affect the potency and performance of your platelets.
Selected platelet donations – why are you special?
- What is a tissue type?
Your ’tissue type’ is also known as your HLA type. It is one of the ways that your body’s defence system identifies the differences between your own cells and foreign cells. - What is HLA (Human Leucocyte Antigen)?
Antigens are proteins, often found on the surface of cells. Antibodies are formed by the body when it recognises a ‘foreign’ antigen. This is part of the body’s defence mechanism against ‘foreign invaders’. These antibodies will destroy ‘foreign’ antigens and the cells they are on. The surface of almost all cells including white blood cells and platelets (but not red cells) carry a set of antigens called Human Leucocyte Antigens (HLA). - Your HLA antigens are determined by the HLA genes you inherit from your parents. There are a number of these HLA genes in various combinations that make up your HLA type, consequently there are thousands of different HLA types in the population. Some HLA types are found in populations throughout the world whilst others are found more commonly in particular ethnic groups.
- Who needs selected (HLA matched) platelet donations?
Patients who require multiple platelet transfusions, such as people with leukaemia, those on long term chemotherapy or with platelet disorders, may develop antibodies to platelets that have different tissue types (HLA) to their own. This means that the patient’s antibodies will destroy any platelets that are different from their own, as a consequence the platelet transfusion is ‘rejected’ and the transfused platelets are destroyed. - When a patient has developed HLA antibodies, we have to select donors who have an HLA type that matches the patient’s own HLA type and that is not seen as ‘foreign’ to the patients immune system.
- Not everybody develops antibodies and the reasons why this happens are not always understood but patients who receive more platelet transfusions are more likely to develop antibodies. The majority of patients don’t have antibodies that destroy platelets and so don’t need to be matched.
- Patients often need platelets unexpectedly and at short notice. The life of a platelet is very short and some patients often need platelets every day or every other day in order to prevent serious bleeding. We must maintain a stock of platelets with a variety of HLA types at all times to ensure we can provide them for patients whenever they are needed.
- Why is HLA type important?
When a patient has a platelet transfusion the transfused cells may be seen as foreign and produce antibodies against the HLA type. In patients that have repeated transfusions the likelihood of producing antibodies increases. - If a patient makes antibodies to an HLA type then platelets have to be selected (or matched) so they are similar to the patients HLA so the antibodies will not recognise them as foreign. If the transfusion isn’t matched then the platelets will be destroyed by the patient’s antibodies before they have a chance to work by stopping or preventing bleeding.
- Finding a perfect HLA match is not always possible for some patients for a number of reasons. In these cases we select the best match we have. Donors who have an HLA type that is homozygous will match more people and therefore their platelets are more likely to be selected for these patients.
- The majority of people have 4 different HLA antigens which make up the tissue type on their platelet but some people have only 2 or 3 antigens. Platelets from donors with 2 or 3 antigens will match many more patients than those with 4 antigens. These donors are called “homozygous” and because they match many more patients they are called “high-value” donors. HLA selected platelets from homozygous donors are less likely to trigger antibody production after transfusion, or be attacked by antibodies that already exist in the patient.
- Why is homozygous “high value”?
Homozygous donors are rare and although different homozygote tissue types will occur at different frequencies on average only 1 in 200 donors are homozygous. - What does this mean for me?
If you are found to be either homozygous then your donations are extremely useful for certain patients. It has no implication to you directly as everybody has an HLA type. We just wanted you to know how your donations are especially needed.
We hope you are able to continue donating as an apheresis platelet donor as often as you are able. - Further information can be found at the NHSBT or by clicking here.
 Click here to find out how to become a platelet donor.
Click here to find out how to become a platelet donor.
Platelets given by generous and committed donors are often life-saving and special in that they can help up to 3 adults or even 12 children.
